Diagnosing Genital Herpes -
How Do You Do It?
Steps to a Diagnosis
There are two general approaches to diagnosing genital herpes:
- Laboratory tests
- Physical exam and history
Laboratory tests can be used to detect the virus directly from skin lesions. A swab is rubbed over the sore and the material on the swab is sent for one of several tests called culture, FA, or PCR. Another test called serology can show evidence in the bloodstream for the patient's immune response to herpes infection. Both virus detection and serology can help confirm the health care provider's suspicions by physical exam and history that infection with genital herpes may have occurred. Genital herpes is common but it is difficult to diagnose just by physical exam and history. Most authorities feel an accurate laboratory test should be utilized to establish the diagnosis.
Laboratory Testing - Overview
Testing for the virus directly from the skin is useful if genital symptoms are present at the time of an office visit to a health care provider. Diagnosing herpes by just looking at a lesion or sore does not give an accurate diagnosis because many other infections or irritations can look just like herpes. As such, and because HSV is a chronic disease, confirmation of the diagnosis with a laboratory test is recommended by almost all medical authorities and by the Centers for Disease Control. When lesions or sores are present the physician or health care provider can swab the sore and submit the sample for detection of herpes simplex virus by growth in culture or by detecting parts of the virus in the material on the swab. Finding the HSV virus by any of these assays shows that HSV caused the lesion.
The one exception to this is that persons occasionally have more than one infectious agent in a single lesion (a "dual" infection). This may include HSV and another organism such as syphilis. In the United States, dual infection is quite uncommon. Dual infections are more common in some other areas of the world.
Another way to diagnose herpes is to detect antibodies in the blood that the body has made to fight off the virus after infection. These antibodies last for a lifetime after an infection. They can be detected by a blood test even if no signs or symptoms are present at the time the patient visits the doctor. Antibodies develop even when patients have never had symptoms of herpes.
Blood tests to identify antibodies are called "serology". Serology can help show that herpes infection has occurred in situations where it is difficult to obtain or to properly transport a sample for virus detection tests. If performed correctly, antibody tests can identify a person as having had an HSV-2 infection or an HSV-1 infection, or both viruses sometime in the past.
HSV blood tests are confusing to patients and to clinicians as well. Unfortunately there are many claims about blood tests--some less accurate than others. This has led to confusion about when blood tests should be done and which tests are accurate. This area of testing is so important, we have devoted an entire section of this website to providing the most current information on HSV serology. Click here to read more about HSV type specific serology.
We have given an overview on the laboratory tests to use for diagnosis. Much more information is given in separate sections below on Viral Culture, HSV FA, Viral PCR, and Serology. There are other things a health care provider can and should consider in evaluating a person with genital lesions, sores, or recurrent symptoms that could be due to herpes.
Physical Exam - Seeing Your Health Care Provider
Consultation with a physician or other health care provider is an important step in getting an accurate diagnosis for herpes. There are laboratories that provide some HSV serology tests on site. However, only a clinician can prescribe effective antiviral medication for herpes. A clinician also knows other parts of your medical situation that might be important. Your visit should include a careful history as well as an examination.
Taking a History: Your health care provider will probably start by asking you for details regarding what brought you into the office. A major part of this, naturally, is to review what symptoms you are having right now but he or she will also want to know if you have experienced these or similar symptoms before. He or she will also ask questions about your sex life, such as how many partners you have had, if you have changed partners recently and whether you use condoms. Some of this may strike you as quite personal, but it's important in determining what further tests to do and, ultimately, in making a correct diagnosis.
The Visual Exam: In addition to taking a sexual history, your doctor will need to perform a thorough examination, including visual examination of the genital area.
For men, the exam usually includes a close look at penis, scrotum, and rectum, looking for blisters or skin lesions characteristic of herpes. Discharge from the urethra is another possible sign of herpes. The clinician might also swab the urethra and anus for a laboratory test.
For women, the current standard of care is to perform a pelvic exam using a speculum to gently hold the vagina open so that the cervix and vagina can be inspected. The clinician should also carefully inspect the labia and the area between the vulva and anus for signs of infection. Swabs of the cervix and anus might be taken for a laboratory test.
For both men and women, the health care provider also should check the lymph nodes, especially those in the inguinal or pelvic region because swollen lymph glands often accompany herpes blisters or skin irregularities.
A visual examination is only one part of a complete diagnostic work-up. Making a diagnosis of genital herpes by visual inspection and by asking you questions is not easy and even experts can be wrong. For one thing, genital herpes doesn't look the same in every patient; it can "mimic" the appearance of other sexually transmitted diseases (STDs) and other STD's can look like herpes.
A mild case of herpes can easily be mistaken for something that has nothing to do with STDs such as a pimple, an ingrown hair, or a simple rash. Thus confirming a diagnosis with a laboratory test is critical.
If your health care provider sees any genital lesions, you should ask if this could be herpes and ask if he or she has ordered a laboratory test for herpes. Most authorities and the Centers for Disease Control feel that laboratory tests are important to be sure that what looks like herpes really is herpes. On the other hand, we do not recommend a swab test (for virus detection) if lesions are not seen. In this situation, we recommend asking for a herpes antibody test.
What if I have symptoms now? What do I do?
Because herpes lesions heal themselves due to your immune response, if you currently have symptoms that you think are related to herpes, you should be examined as soon as possible by a medical professional and should also request one of the laboratory tests described below.
Click here to go to the symptoms section.
The earlier you see your health care provider, the better. When signs and symptoms are present your medical professional has a better chance to examine them. Also he or she may be able to swab a sore or tender area of skin, genital region, or rectal area for a laboratory test to detect herpes virus. If too much time passes before you are examined by a clinician, physical signs of infection like swollen glands may be disappearing and any sores or areas with virus may no longer contain large enough amounts of virus to provide a good sample for testing.
What if I had symptoms a while ago but they've gone away?
The best way to tell if you have had herpes in the past is with a type specific HSV serology or antibody test. This test can't tell you if the particular symptoms you had recently are due to herpes but if your test is positive for HSV-2 antibodies, your health care provider can help teach you to recognize symptoms so that virus detection tests can be done at the time symptoms come back. Viral culture, antigen detection, and PCR are the only tests that can show if an area of pain or irritation in the genital or rectal area is being caused by the presence of herpes at the time of swab sampling.
More About Laboratory Tests
Testing for the virus directly from the skin is useful if genital signs or symptoms are present at the time you are examined. When lesions or sores are present the physician or health care provider can rub the sore with a swab and submit the sample for detection of herpes simplex virus. There are three main ways laboratories detect HSV from swabs:
Viral Culture
HSV-1 & HSV-2 grow in what is called tissue culture cells or "cell culture." When changes in the cell culture are seen under a microscope, the laboratory does further tests to show that the changes are due to HSV and that the virus is HSV-1 or HSV-2.
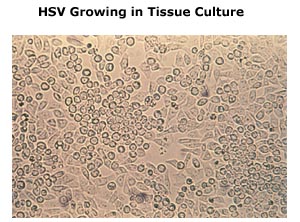
This picture was taken through a microscope to show cells that have rounded up due to HSV infection. Isolation of HSV from a sore by growth in cell culture is definitive proof that HSV caused the sore.
However, viral culture can take 1-10 days to become positive and even a good sample taken from a lesion with herpes may be negative.
Some laboratories use a version of viral culture called "shell vial" culture to make the test faster (only 1-2 days) but this test is not as sensitive as standard viral culture. This means the shell vial test has a higher chance than standard culture of being negative even though herpes is present.
An interesting version of viral culture is called the ELVISTM-Id test. ELVIS stands for "enzyme-linked virus-inducible system." This test uses special cells created to contain the genetic code for an enzyme unrelated to herpes. When HSV from a patient's swab infects the ELVIS cells, this enzyme is switched "on" and causes the cells to turn blue. This photo shows ELVIS "blue cells" surrounded by uninfected clear cells.
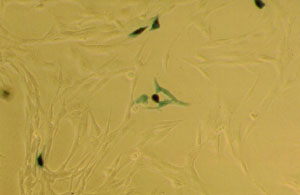
A number of commercial laboratories use this test. It is likely to cost more than a standard culture. ELVIS tests may miss some cases of herpes either because there is so much virus in the sample that the cells are destroyed before the test can be completed or because there is very little herpes in the sample. ELVIS tests are usually completed in 1-2 days.
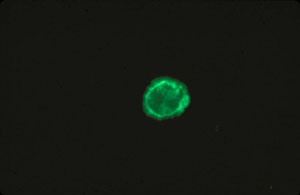
HSV Fluorescent Antibody Test ("HSV FA")
Fluorescent antibody techniques (FA) are faster than culture and nearly as sensitive for lesions that have newly formed. These tests are less accurate for older, healing lesions. Occasionally, FA can be more sensitive than culture if the virus has not survived transport. One study showed that the most accurate approach is to do both a viral culture and FA test. This cell is positive for HSV-2.
Viral PCR
PCR or "polymerase chain reaction" tests are the most accurate tests for herpes. PCR techniques make many copies of the viral genetic material (DNA) in a short time so that even tiny amounts of virus are sufficient for a positive test. Only about 4 hours is needed once the specimen arrives in the lab. PCR can tell if HSV-1 or HSV-2 is present. PCR is more expensive than culture but may be the only test sensitive enough to find herpes in a lesion that does not contain much virus.
This chart shows how much more sensitive PCR can be than culture. Of over 36,000 specimens that were tested by both culture and PCR, 3377 were positive by PCR but negative by culture. A lot of the specimens that were positive only by PCR were collected in warmer summer months. Warm transport conditions can harm the virus so that it can't infect culture cells but PCR tests are unaffected. This is another reason PCR is more accurate than culture.
PCR Test Result
| Culture Result | Neg | Pos | Total Specimens |
| Neg | 32,007 | 3377 | 35,384 |
| Pos | 49 | 1038 | 1087 |
| Total Specimens | 32,056 | 4415 | 36,471 |
|
Should I ask for a PCR or a culture?
At this time, PCR is less available and more expensive than culture or FA. But PCR is more likely to give you a correct answer. The chance of missing herpes in a lesion by culture or FA is much higher than with PCR. If PCR is not affordable or available to you, a type specific serology blood test is good alternative to see if you have been infected with HSV.
Other Tests for Herpes
Some clinics will use diagnostic tools other than the tests we have covered here. Two that are generally not recommended are the Tzanck test and the Pap smear, neither of which is very accurate. A positive test by these methods may be due to a virus that is not herpes. A negative test does not mean herpes is not present.
My provider recommends regular Pap tests. Why?
A Pap smear is designed to look for early changes that might be related to cervical cancer. Most medical authorities recommend regular Pap tests. Talk to your provider about how often you should get a Pap test.
The New Blood Tests ("Type-Specific Serology")- An Overview
The most important breakthrough in herpes diagnosis in the last few years is the development of serology tests that accurately tell you if you are a carrier of HSV-2.
Serology tests detect "antibodies" in the blood. These are substances produced by the immune system to fight off infection. If antibodies are found in the blood, it means your immune system has seen herpes virus infection in the past and fought it off. It also means that HSV is dormant in your nervous system and you are a carrier of the virus. Blood tests obviously don't require swabbing a lesion, so they can be done long after symptoms have faded.
The key to accuracy for herpes blood tests is to make sure that the test is a 'type-specific' assay that can tell the difference between HSV-1 and HSV-2 antibodies. Many commercially available tests currently cannot make this distinction despite their claims. Thus, you need to ask your health care provider if they sent your blood to a laboratory that does one of the "new" glycoprotein-G herpes antibody assays. These tests are covered in detail in the section on blood tests.
Serology testing is better than culture or antigen tests at telling whether a person has had an HSV-2 infection, but there are two things you should know. The first is timing: If this is a new infection with herpes, a person may take several weeks to three months to develop the antibodies. The second is that some blood tests cannot tell the difference between the two types of herpes, HSV-1 and HSV-2. Unfortunately, not all laboratories and not all doctors are aware of the new blood tests. More importantly, lots of old style blood tests are still being done. For this reason, anyone seeking an accurate diagnosis of genital herpes must be sure to get a "gG-based type-specific" serologic test.
One reason we founded this web site is to try to inform people about the correct serology tests to use. We will tell you more about these new tests in the next few screens.
Type-specific antibodies. The new blood tests are based on antibodies to two proteins that make up part of the HSV-1 and HSV-2 virus structure.
- One protein is called glycoprotein gG-1 and it is found only on the outside of the HSV-1 virus or in cells infected with HSV-1 as the virus is produced.
- The other protein is called glycoprotein gG-2 and is found on HSV-2 virus or in cells infected with HSV-2.
These proteins have similar names but they are enough different that antibodies that are produced to one HSV type (say, HSV-1) cannot be mistaken for the other type (HSV-2) in the new serology tests. We call antibodies that can react to only one, not both, HSV types "type specific."
Isn't gG a kind of antibody?
The short name for "glycoprotein G" is a common source of confusion. The main antibody to develop in response to infection is called Immunoglobulin G or "IgG". When scientists were working out the structure of herpes virus, they named the viral glycoproteins alphabetically in order of their discovery.
Thus, gG was the seventh glycoprotein to be discovered. As shown in the diagram, other glycoproteins such as gB and gD are also on the outside of the virus.
In herpes infections, people make gG antibodies against gG-1 or gG-2
gG-1 and gG-2 Based Blood Tests
It is very important that a blood test be based on detecting antibodies to gG-1 (for HSV-1 infection) or gG-2 (for HSV-2 infection). Tests that combine many HSV proteins without singling out gG have a high chance of missing HSV-2 antibodies in people who are infected with HSV-2 or giving a positive test for HSV-2 antibodies when the person has been infected with only HSV-1. This type of inaccurate result can be confusing for health care providers and very distressing for patients.
It is possible and very common to have a positive test for antibodies to one type of gG (say, gG-2) and a negative test for the other type (gG-1). Blood can have antibodies to HSV-1 only, HSV-2 only, or both HSV-1 and HSV-2.
For details on how to get an accurate gG-based blood test, click here.
What if I had symptoms before but now they're gone? Can I still get tested for herpes?
Lots of people need to be tested more than once. As we explained above, one of the most widely used tests for herpes is the viral culture and it often misses herpes even when the virus is present. Often a patient who has received a negative culture result will be asked to come back again when a new lesion appears so that culture can be tried a second or third time.
In contrast to this approach, one of the new gG-based, type specific blood tests is more efficient, since it can find antibodies to herpes anytime after the first few weeks of infection. With these tests, you don't need to wait until you have signs or symptoms before you go in for testing. You just need to be sure you have waited long enough after first becoming infected so that your body has developed antibodies.
Type-specific blood tests are ideal for those who have had a history of genital symptoms but have never had a successful laboratory test for herpes.
What if I've never had symptoms before but want to know for sure?
If you've never had symptoms before but want to be tested for herpes, a type-specific blood test is the only way to find out your status. Getting tested may make sense if you:
- Are in a relationship where your partner has herpes.
- Have had several sexual partners and want to be screened for the most prevalent STDs.
- Have had another STD in the past and wonder if you might have acquired herpes also.
A blood test also can be useful information for women undergoing prenatal screening. For more information about herpes in pregnancy, click here.
Are all HSV type specific serology tests based on gG?
No. A number of tests claim to be type specific because they have two parts--an HSV-1 part and an HSV-2 part. This alone is not enough to detect antibody to HSV-2 in those infected with HSV-2 but not in people that are infected with only HSV-1. Some laboratories still use these tests. A list of laboratories that use accurate tests is available in the section on blood tests.
Advantages and Disadvantages of Laboratory Tests
| TEST TYPE |
SPECIMEN SOURCE |
ADVANTAGES |
DISADVANTAGES |
| Viral Culture |
Swab of lesion |
Highly specific Widely available |
-Sensitivity a function of specimen quality/ timing -Virus must be kept alive during transport to the lab |
| ELVIS Culture |
Swab of lesion |
Highly specific Rapid; 1-2 days |
-Can be falsely negative -Expensive |
| Antigen Detection |
Swab of lesion |
Rapid; less than 1 day; inexpensive |
Sensitivity lower than culture |
| PCR | Swab |
Very sensitive |
Not widely available; still expensive |
| Type-Specific Serology (gG-based) |
Blood draw Some use finger-stick |
Test can be performed in absence of lesions Highly accurate. |
-Need time for antibodies to develop days post infection; -Tests that are not gG-based have inadequate accuracy. |
| Serology not gG-based |
Blood draw |
Not recommended |
Not recommended |
|