What About Herpes and Pregnancy?
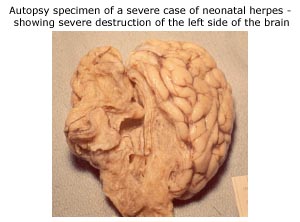
One of the major concerns about genital herpes is the problem it places in pregnancy. Herpes virus type 1 and type 2 can be transmitted to the infant. This invariably occurs at the time of delivery. Infants who acquire HSV so early in life do not have mature immune systems and hence the herpes viruses can get into brain tissue and spread throughout the body. In the pre- antiviral days newborns with herpes usually died. Now with antivirals only 5% die, but many suffer brain damage. This is why preventing this from happening is critical. The new antibody assays to identify persons can be very useful in this regard. Paradoxically, it is women who do not have herpes, but who acquire it in the late 3rd trimester that are at greatest risk of transmitting herpes to the infant.
In some cases herpes is transmitted to infants at the time of delivery if the baby comes into direct contact with herpes on the way through the birth canal. Herpes infections in newborns are rare, but they can be life threatening. For this reason, pregnant women and their partners are well advised to take steps to keep this risk to a minimum.
If you already have genital herpes: If you had genital herpes before you became pregnant, your risk of transmitting the infection to your baby during childbirth is low as long as no active herpes signs or symptoms are present in or near the birth canal at the time of delivery.
If no signs or symptoms of herpes are present when you go into labor, you can expect to have a normal vaginal birth. Women who have long standing herpes infections transmit protective antibodies to their fetuses during pregnancy. The antibodies help to protect the baby from an infection, even if some virus is present in the birth canal. Most doctors obtain a culture of HSV-2 seropositive women at the time of delivery. About 2% HSV-2 seropositive women shed virus at delivery and potentially expose the infant. However, less than1% of these babies get newborn herpes. Thus, less than 1 of every 100 infants born to mothers with HSV-2 are at risk of developing neonatal herpes. So, if an exposure occurs the baby is closely followed.
If you do have signs or symptoms of herpes when you start labor, your doctor will deliver your baby by cesarean section (abdominal delivery). This will protect your baby from exposure to the large quantities of virus that are likely present in the birth canal or on the skin during a herpes outbreak.
If you do not have genital herpes: If you have never had genital herpes, you will need to take steps to ensure you do not get the infection during your pregnancy. A woman who gets herpes for the first time while pregnant has a significant risk (33-50%) of transmitting the virus to her baby during childbirth. One reason for this is the relatively high rate of viral shedding in the first six months after acquiring infection. Another is the fact that the mother will not have developed her immune response to herpes, including the antibodies that are passed to the fetus in utero.
Women who have a partner with genital herpes, but who are HSV-2 negative are at particularly high risk of acquiring HSV-2 near delivery and, hence, transmitting it to their infant.
Thus, if your husband or partner has genital herpes, your doctor may recommend that you use condoms every time you have intercourse throughout your pregnancy. In addition, your doctor may recommend that you abstain from intercourse during your last trimester, which is the most dangerous time to develop a first-episode infection. Lastly, genital herpes type-1 can be transferred by oral-genital sex from partners with histories of cold sores. Therefore, it is best to also avoid oral-genital sex during this time period.
If you become infected in the first trimester, vaginal delivery may still be possible. With a new infection after the first trimester, however, your doctor may elect to deliver your baby by cesarean section whether or not active herpes signs or symptoms are present at the time of delivery. Your doctor also may recommend antiviral medication during pregnancy. This is because your risk of reactivation is high and you may not transmit all the protective antibodies needed to prevent neonatal herpes.
If you acquire primary herpes during pregnancy: Women with primary infection at any time during pregnancy should be treated with antiviral therapy. If you acquire genital herpes near delivery some clinicians recommend treatment with antiviral medications until delivery, some recommend Cesarean delivery, and other recommend both. Your doctor should discuss various management options with you and your partner.
How can a blood test be used during pregnancy?
Because the highest risk of neonatal herpes occurs when a woman acquires herpes during pregnancy (particularly near term), some experts advocate testing to find out whether a woman is at high risk. Some experts recommend that all women get a type specific serologic test at the 28th week visit. Women who lack antibodies to either HSV-1 or HSV-2 (seronegative) should avoid either oral genital or unprotected coital activity in the last month of pregnancy. This is particularly important if the partner is seropositive for either virus or if his serostatus is unknown. Attempts should be made to assess serostatus of the partner whenever possible.
If you are HSV-1 (without a history of cold sores) or HSV-2 seropositive, then you should be counseled, offered management options, and examined for carefully lesions at delivery. Some clinians have used valaciclovir 500 mg twice a day or acyclovir 400 mg three times a day from thirty-five weeks to delivery. All women should be examined carefully at delivery for lesions and, if lesions are present, a Cesarean delivery considered.
What are the signs of herpes in a newborn?
Skin sores, fever, listlessness and lack of appetite are among the early symptoms or neonatal herpes. Without prompt treatment, brain or nervous system damage may occur, and some babies will die from this infection.

While herpes infection can be devastating to a newborn, it is rare. Nearly one in every three women of childbearing age in the United States today has the virus that causes genital herpes. Yet fewer than 1 in every 2,000 newborns born to such a woman develops the infection. Good prenatal care may reduce this already small risk even further. However, since the interval between birth and diagnosis of neonatal herpes has not changed in the last twenty years, identification of who is at risk of transmission is imperative. Once identified, the pediatrician can be alerted to the potential risk of neonatal herpes.